NHS in Shropshire special report: What lies ahead for the county's healthcare?
Today, the Shropshire Star embarks on a week-long study into the future of NHS services in Shropshire.
It was supposed to guide the future of Shropshire's health services for generations to come.
Dubbed Future Fit, leading professionals were to come together, decide how the NHS should work and come up with a plan.
But the whole exercise has been delayed after becoming bogged down with arguments, money concerns and resignations.
Today, the Shropshire Star embarks on a week-long study into the future of NHS services in Shropshire.
1: £294 million
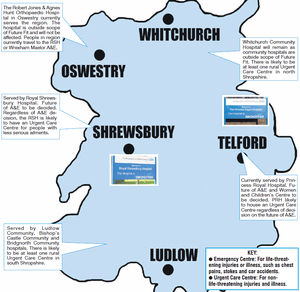
Option one, costing £294m, would see Telford's Princess Royal Hospital housing the county's only A&E department, along with an urgent care centre, local planned care and obstetrics.
Royal Shrewsbury Hospital would lose its A&E department, but would provide a diagnostic treatment centre, an urgent care centre and local planned care.
2: £354 million
Royal Shrewsbury Hospital would house the county's only A&E department, along with an urgent care centre, local planned care and obstetrics.
Princess Royal Hospital would lose its A&E department, but would provide a diagnostic treatment centre, an urgent care centre and local planned care.
3: £280 million
Royal Shrewsbury Hospital would house the county's only A&E department, along with an urgent care centre and local planned care.
Princess Royal Hospital would lose its A&E department, but obstetrics would remain along with diagnostic treatment centre, urgent care and local planned care.
We kick off with a look at the options facing the county and the probable outcome of the Future Fit consultation. Through the week we will take a look at how a reorganisation of A&E would impact on parts of our region.
One issue appears to be clear: Shropshire will lose one of its A&E departments from either Shrewsbury or Telford. The remaining A&E will be supported by a number of urgent care centres scattered across the county. The costs of each option range from an estimated £280 million to £354 million.
The key question of course is this: Should Telford's Princess Royal Hospital or the Royal Shrewsbury lose its A&E? And what does the decision mean for people living in outlying areas who face long journeys to hospital in the event of an emergency?
The decision was meant to be taken this autumn, followed by a period of public consultation. It has now been put off until next year, although the Future Fit team insist they continue to work towards a solution.
The background to this involves concerns that any solution will not adequately tackle the growing £23 million deficit of Shrewsbury & Telford Hospitals NHS Trust, which runs our two main hospitals.
And there has been chaos at Shropshire Clinical Commissioning Group, which runs services in Shropshire borough and is an important part of the Future Fit process. Its accountable officer Dr Caron Morton has resigned from her role and the group has effectively been placed in special measures after forecasting a £10.6 million deficit.
Enter David Evans, chief officer of Telford & Wrekin Clinical Commissioning Group, whose job is to pick up the pieces of Future Fit and move it forward.
The pressure is on, especially as around £3 million is being spent on a process that has so far come up with no answers.
But he insists this is not simply a cost-cutting exercise for the NHS. His team also has a duty to ensure that every part of the county has the skills it needs to ensure patients are safe.
Future Fit began in 2012 after NHS England set out a 'call to action' to staff, public and politicians to help the NHS meet future demand and tackle funding gaps through 'honest and realistic' debate.

Mr Evans said: "NHS England wanted us to engage with the public around how to make sure the NHS stays sustainable over the coming decade.
"Clearly there are significant challenges the NHS is facing, not just around money but also around clinical sustainability.
"We locally ran a call to action campaign jointly with the two CCG's – Shropshire and Telford & Wrekin.
"We had a lot of responses from members of the public.
"We ran a conference in November of that year at the international centre to look at what this might mean.
"There were some key messages coming from members of the public around what they thought needed to be done.

"There was a clear message that no change was not an option – they wanted to change.
"There was clear message that clinicians needed to be heavily involved and to make sure this was clinician lead.
"So arising out of that the two CCGs asked some clinicians to go away into a darkened room and come up with a clinical model that covered emergency care, planned care and long term conditions.
"That group of clinicians – amounting to 300 including doctors, nurses, paramedics and social workers – presented us with a clinical model of what they thought care in the future should look like.
"That happened 18 months ago.
"The start of the clinical model was the start of Future Fit. We were very clear this was about how we transform services for the population and we were very clear the Future Fit programme covered acute and community hospitals, community services, mental health care and primary care.
"As you will know for some time the acute hospital has struggled to recruit consultants particularly in key areas like A&E – it has struggled to recruit other staff as well.
"We were very clear that the focus of anything we came up with was to make sure that it was the right model to deliver good quality care for the future but make sure that we had the right staff to deliver it.
"So in essence that is where we started."
Mr Evans said one of the main reasons health services in the region needed to be redesigned was to consolidate the staff they currently had and to attract new consultants.
He added: "I believe we are still looking at the 999 life-threatening cases to be taken to one place.
"I think the notion of about 75 per cent of what currently goes to A&E should be seen in urgent care centres.
"I would never rule anything out. But it will be one emergency centre supported by other centres. All that will be underpinned by patients being looked after closer to home.
"The biggest difference with Future Fit is that it will enable us to have the right clinicians in the right places to give the right care.
"At the moment we are very spread out."

Mr Evans admits the issue is a juggling act and that there are immediate issues to tackle alongside the longer-term Future Fit programme.
He said: "Some things need to be sorted before Future Fit, such as A&E performance targets. We need to bring that down by March.
"It is tough and the hospitals are full. It is difficult at the moment.
"It ought to be easier. The current A&E times are not good enough.
"There is a general consensus that we have to do this. If we don't we will end up having to cut services. We just need to change the way we think.
"I am very optimistic about this, if we come up with the right solution.
"We hope to come up with a preferred option by June."
The delay to Future Fit happened because none of the options on the table adequately tackled the growing £23 million deficit of Shrewsbury & Telford Hospital NHS Trust (SaTH).
Mr Evans said: "If I looked at other transformation programmes within the NHS, they have been financially driven not clinically driven – so you are dammed if you do and dammed if you don't.
"We wanted to make sure it was the right model for patients rather than being financially driven.
"Of course you have to make sure those two marry up and you can do that. It is a bit like going to buy a car – in simplistic terms. If I went into a garage today to buy a car and was offered climate control, DAB radio, sat-nav, etc I would take it but you get to the stage where you cannot afford that now and look at scaling that back.
"So this is now about saying the clinical model is right and we agree with that.
"The issue is how do we make that clinical model work with the money we have got to deliver the best care for patients.
"We are now having discussions about how much of the wish-list is essential and how much is desirable and can we take things out there. We are having discussions about ways we can do things more efficiently, more cost effectively without reducing the quality.
"If you get the quality of care right you take the waste out of the system. SaTH at the moment is working with the Virginia Mason Institute to look at what they have been through and I was privileged to recently be in Seattle with the SaTH team looking at that.
"We have to take some waste out of the system because undoubtedly there is some.
"A prime example of that at the moment is we have significant challenges around A&E waiting times and we are struggling to meet the four-hour target.
"If we completely change the ways we worked around hospital care that might mean we have fewer hospital admissions.
"Most of the capacity that SaTH has opened to deal with the pressures is to a large extent staffed by agency and locums and they are very expensive.
"To take some of that away you would make a relatively quick saving without impacting on patient safety.
"The programme has a temporary pause to it but work is still going on."





