Colleagues in tears and night panics – ICU doctors describe coronavirus despair
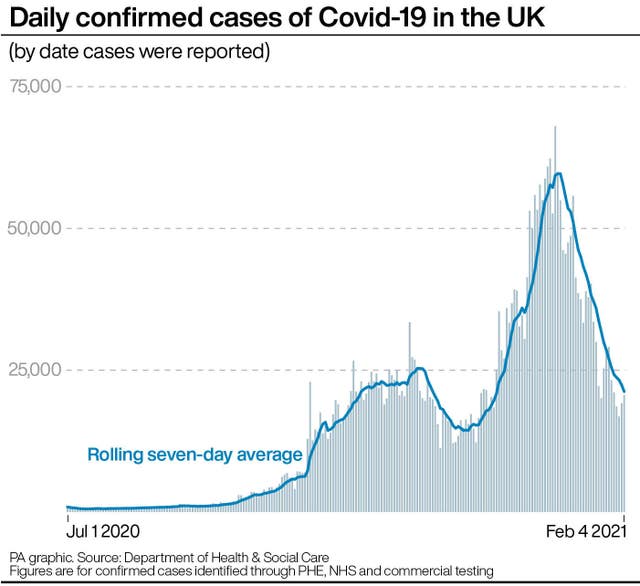
Although lockdown has brought a dramatic drop in cases, some intensive care units are yet to see the same fall in patient numbers.

Intensive care doctors have described jolting awake at night and witnessing colleagues breaking down as they warned that specialist units are “not out of the woods” with coronavirus cases.
Despite a downward trend nationally in coronavirus cases and hospital admissions, consultant Dr Ben Attwood said intensive care units such as his at Warwick Hospital are yet to see the same level of reduction.
He told the PA news agency that staff will not be able to cope if policy-makers “take their eye off the ball” and remove restrictions too quickly.
Dr Attwood, 43, said the delay between transmission of Covid-19 and the deterioration of patients’ conditions means his hospital is still seeing people “who might have been infected in the Christmas period and just after”.
“It’s rare at the moment to get through a shift where a member of staff isn’t on the verge of or actually in tears. That’s really unusual,” said Dr Attwood, who is associate medical director at South Warwickshire NHS Foundation Trust.

“We absolutely are not out of the woods. Whilst it’s really tempting to say we can now take our eye off the ball, we absolutely can’t.
“If we lose our focus now and people start to let up – and I don’t just mean public, I mean government – we are in danger of just essentially Groundhog Day of lockdowns and cycles.
“I don’t think the NHS is ready to cope with that. I just don’t think there’s enough fuel in the tank.”
Another ICU doctor from London, who wished to remain anonymous, told PA: “We expect to remain full with high demand for at least the next few weeks.
“A lot more help is needed, especially in critical care. The last year has been utterly relentless, and the vast majority of us are experiencing effects on our mental health.
“I’ve never had a single issue with stress, anxiety or anything like that and yet even I find myself waking up regularly in the night with jolts of adrenaline as if I’m still on the intensive care unit and there’s another emergency.”
As a smaller medical centre, Dr Attwood’s Warwick Hospital only had funding and staff to treat five critical care patients in 2019, but as with hospitals across the country it has doubled its capacity during the pandemic – treating as many as 13 at a time.
“In a larger hospital that would sound very small, but along with a small bed base you also have a very small nursing and medical staffing facility,” he said.
“If you’d said to me two years ago that (Warwick) would have more than double the actual physical number of beds available I’d have looked at you like it was madness.”
Dr Attwood said the difficulties staff are facing are exacerbated by the fact many have been redeployed to intensive care, but all staff are under intense strain.
He said colleagues are not being afforded the usual time and energy to recover from the trauma of their experiences in ICUs.
“Intensive care staff are in usual times incredibly well placed to deal with this and extremely professional, but I think this has taken its toll on everybody,” he said.
“The way in which nurses and medics normally can bounce back and deal with and start to process the enormity of what they’re doing usually involves debriefing either formally or informally.
“The trouble with this particular pandemic is there isn’t that opportunity.
“It can be as simple as having a cup of tea with somebody or meeting people informally (outside of work) – and of course we’re not allowed to do that.”





