Senior medic defends remote GP appointments, saying ‘pandemic isn’t over’
GPs have come under fire in the media for not offering enough face-to-face appointments.

The head of the Royal College of GPs has defended doctors who are still opting for remote consultations, saying the “pandemic isn’t over”.
Professor Martin Marshall, chair of the college, told the Health and Social Care Committee that some patients preferred appointments over the phone or via video, while others wanted to be seen face-to-face, but could not be due to Covid.
He said about 80% of general practice appointments were conducted face-to-face prior to the pandemic, dropping to 10% in the first wave and now sitting at about 56%.
He told MPs that 56% was “where we should be” adding that face-to-face appointments “aren’t needed by everybody” and “I don’t think we’re going to go back to 80% of consultations in general practice being face-to-face”.
He also said: “What we’ve learned from the pandemic is we can do more in general practice remotely than we thought we could, and that’s a positive bit of learning.
“There’s a lot of stuff that can be done without having to examine someone or be in the same room.
“Having said that, face-to face-contact is a really important part of dealing with, particularly, more complex problems.”
Prof Marshall said there were three categories of patients who needed to see GPs.
“There’s people who like and get real benefit from remote care, there’s patients who absolutely need to have face-to-face contact in order to get the high quality care to pick up the right diagnosis – not just examining but for picking up soft signs – and then there’s a large group of people in the middle who would like to have face-to-face care, but general practice currently doesn’t have the capacity to deliver it.
“That’s the bit which is the real problem for patients and for general practice.”
Asked if patients had a right to see a GP in person, Prof Marshall said: “People are saying that the patient should have a right.
“There’s no point in having a right if it’s undeliverable and it is essentially undeliverable at the moment, because of the workload pressures.”
He said GP workload had gone up over the pandemic “and indeed over the last decade”.
And he added: “The second thing is, really importantly, the pandemic isn’t over.
“We’d like to think it is – it isn’t over, it might be over for pubs and nightclubs, it’s not over for health services.
“It’s really important that if you run a health service, whether it be in general practice or in hospitals, that you protect vulnerable patients.
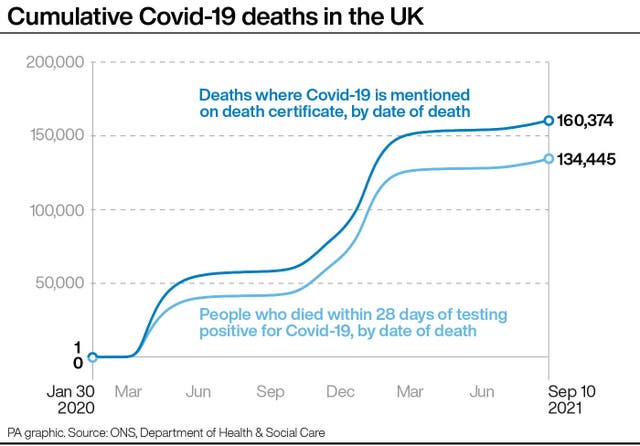
“The prevalence (is) around one in 70 and 80 patients in this country have got Covid, so the idea of having somebody who is fit and healthy but shedding the virus sitting next to someone who’s vulnerable in a waiting room is just not something that’s acceptable.”
Prof Marshall also said the theory that GPs offering remote consultations has pushed up trips to A&E was not supported by evidence, although that may have happened at the height of the pandemic.
Asked by committee chair Jeremy Hunt about people not being able to see their own GP for repeat appointments, Prof Marshall said: “I think the essence of general practice is the long-term relationships that the patients and their GPs are able to develop, that gives you an understanding of people’s health beliefs and allows you to make diagnoses more effectively.
“So this concept of continuity of care has long been something that had been an important part of general practice.”
However, he said “not all patients need continuity all the time”, although there was evidence that people seeing the same GP had dropped over time.
On the reasons why, he said: “Patients are less likely to stay in one place for a long period of time, GPs are more likely to work part-time, more likely to be geographically mobile as well, so there are a lot of societal factors as well as health service factors that have contributed.”
He said there was a need to build the general practice workforce “to get back to general practice being able to deliver more personal care and GP and patients getting to know each other more effectively.
“We’re a long, long way away from that, at the moment.”
He added that people needed to face the reality that many medics, including younger ones, do not want to work full time.
GPs have come under fire in the media for not offering enough face-to-face appointments, with Health Secretary Sajid Javid saying the Government would urge them to do so.
On Tuesday, Dr Richard Vautrey, from the British Medical Association’s GP committee, said the “anti-GP rhetoric in the media risks fuelling a climate of spiralling abuse”.
He added: “GPs are seeing millions of their patients face-to-face, as well as offering telephone and online appointments, every week.
“The move to an initial telephone consultation to assess a patient’s needs was, and is, in line with NHS England’s and the Government’s guidance and is still necessary for infection control and to keep patients and healthcare staff as safe as possible.
“No-one wants to leave a surgery with an infection they did not attend with.
“Many patients have really appreciated the benefit of alternative types of consultations, which can then be followed by a face-to-face appointment if needs be.”
In April, a House of Lords report said the Government must create a hybrid system for the NHS that embraces virtual consultations while allowing face-to-face appointments to continue.
Baroness Martha Lane-Fox, chairwoman of the House of Lords Committee on Covid-19, said the benefits of the move towards digital healthcare seen during the pandemic “are immense” but people who are less digitally able must not be left behind.
The study said “the future will be hybrid” and services will need to be “provided both remotely and face-to-face, with some patients preferring remote services, others preferring face-to-face services, and some preferring a mix of both”.
However, it warned that going digital “can never be seen as a universal solution” because some medical appointments cannot be effectively provided remotely.





